 |
| Shutterstock |
In an uncertain world with conflict, existential climate and environmental impacts and economic unknowns, it's important to find time to find some time for peace, serenity and connection with family and friends.
 |
| Shutterstock |
Contamination of both the general environment and the human population from chemicals has long been a deep concern and for the most part, the issue has been one that can be controlled with the ''its-not-too-late" ethos. For this issue however, that ethos cannot apply.
The US Centers for Disease Control (CDC) provides the basic understanding of the scale of the problem that is now an irreversible contamination of world-wide significance.
The CDC states " The per-and polyfluoroalkyl substances (PFAS) are a group of chemicals used to make fluoropolymer coatings and products that resist heat, oil, stains, grease and water. Fluoropolymer coatings can be in a variery of products. These include clothing, furniture, adhesives, food packaging, heat-resistant non-stick cooking surfaces, and the insulation of electrical wire. Many PFAS, including perfluorooctanoic sulfonic acid (PFOS) and perfluorooctanoic acid (PFOA), are a concern because they:

Antimicrobial resistance is one of the biggest global threats to health, food security and development. This month, The Conversation’s experts explore how we got here and the potential solutions.
These days, we don’t think much about being able to access a course of antibiotics to head off an infection. But that wasn’t always the case – antibiotics have been available for less than a century.
Before that, patients would die of relatively trivial infections that became more serious. Some serious infections, such as those involving the heart valves, were inevitably fatal.
Other serious infections, such as tuberculosis, weren’t always fatal. Up to a half of people died within a year with the most severe forms, but some people recovered without treatment and the remainder had ongoing chronic infection that slowly ate away at the body over many years.
Once we had antibiotics, the outcomes for these infections were much better.
You’ve probably heard of Alexander Fleming’s accidental discovery of penicillin, when fungal spores landed on a plate with bacteria left over a long weekend in 1928.
But the first patient to receive penicillin was an instructive example of the impact of treatment. In 1941, Constable Albert Alexander had a scratch on his face that had become infected.
He was hospitalised but despite various treatments, the infection progressed to involve his head. This required removing one of his eyes.

Howard Florey, the Australian pharmacologist then working in Oxford, was concerned penicillin could be toxic in humans. Therefore, he felt it was only ethical to give this new drug to a patient in a desperate condition.
Constable Alexander was given the available dose of penicillin. Within the first day, his condition had started to improve.
But back then, penicillin was difficult to produce. One way of extending the limited supply was to “recycle” penicillin that was excreted in the patient’s urine. Despite this, supplies ran out by the fifth day of Alexander’s treatment.
Without further treatment, the infection again took hold. Constable Alexander eventually died a month later.
We now face a world where we are potentially running out of antibiotics – not because of difficulties manufacturing them, but because they’re losing their effectiveness.
We currently use antibiotics in humans and animals for a variety of reasons. Antibiotics reduce the duration of illness and the chance of death from infection. They also prevent infections in people who are at high risk, such as patients undergoing surgery and those with weakened immune systems.
But antibiotics aren’t always used appropriately. Studies consistently show a dose or two will adequately prevent infections after surgery, but antibiotics are often continued for several days unnecessarily. And sometimes we use the wrong type of antibiotic.
Surveys have found 22% of antimicrobial use in hospitals is inappropriate.

In some situations, this is understandable. Infections in different body sites are usually due to different types of bacteria. When the diagnosis isn’t certain, we often err on the side of caution by giving broad spectrum antibiotics to make sure we have active treatments for all possible infections, until further information becomes available.
In other situations, there is a degree of inertia. If the patient is improving, doctors tend to simply continue the same treatment, rather than change to more appropriate choice.
In general practice, the issue of diagnostic uncertainty and therapeutic inertia are often magnified. Patients who recover after starting antibiotics don’t usually require tests or come back for review, so there is no easy way of knowing if the antibiotic was actually required.
Antibiotic prescribing can be more complex again if patients are expecting “a pill for every ill”. While doctors are generally good at educating patients when antibiotics are not likely to work (for example, for viral infections), without confirmatory tests there can always be a lingering doubt in the minds of both doctors and patients. Or sometimes the patient goes elsewhere to find a prescription.
For other infections, resistance can develop if treatments aren’t given for long enough. This is particularly the case for tuberculosis, caused by a slow growing bacterium that requires a particularly long course of antibiotics to cure.
As in humans, antibiotics are also used to prevent and treat infections in animals. However, a proportion of antibiotics are used for growth promotion. In Australia, an estimated 60% of antibiotics were used in animals between 2005-2010, despite growth-promotion being phased out.
Bacteria become resistant to the effect of antibiotics through natural selection – those that survive exposure to antibiotics are the strains that have a mechanism to evade their effects.
For example, antibiotics are sometimes given to prevent recurrent urinary tract infections, but a consequence, any infection that does develop tends to be with resistant bacteria.
When resistance to the commonly used first-line antibiotics occurs, we often need to reach deeper into the bag to find other effective treatments.
Some of these last-line antibiotics are those that had been superseded because they had serious side effects or couldn’t be given conveniently as tablets.
New drugs for some bacteria have been developed, but many are much more expensive than older ones.
The concept of antibiotics as a valuable resource has led to the concept of “antimicrobial stewardship”, with programs to promote the responsible use of antibiotics. It’s a similar concept to environmental stewardship to prevent climate change and environmental degradation.
Antibiotics are a rare class of medication where treatment of one patient can potentially affect the outcome of other patients, through the transmission of antibiotic resistant bacteria. Therefore, like efforts to combat climate change, antibiotic stewardship relies on changing individual actions to benefit the broader community.

Like climate change, antibiotic resistance is a complex problem when seen in a broader context. Studies have linked resistance to the values and priorities of governments such as corruption and infrastructure, including the availability of electricity and public services. This highlights that there are broader “causes of the causes”, such as public spending on sanitation and health care.
Other studies have suggested individuals need to be considered within the broader social and institutional influences on prescribing behaviour. Like all human behaviour, antibiotic prescribing is complicated, and factors like what doctors feel is “normal” prescribing, whether junior staff feel they can challenge senior doctors, and even their political views may be important.
There are also issues with the economic model for developing new antibiotics. When a new antibiotic is first approved for use, the first reaction for prescribers is not to use it, whether to ensure it retains its effectiveness or because it is often very expensive.
However, this doesn’t really encourage the development of new antibiotics, particularly when pharma research and development budgets can easily be diverted to developing drugs for conditions patients take for years, rather than a few days.
If we fail to act, we are looking at an almost unthinkable scenario where antibiotics no longer work and we are cast back into the dark ages of medicine – David Cameron, former UK Prime Minister
Antibiotic resistance is already a problem. Almost all infectious diseases physicians have had the dreaded call about patients with infections that were essentially untreatable, or where they had to scramble to find supplies of long-forgotten last-line antibiotics.
There are already hospitals in some parts of the world that have had to carefully consider whether it’s still viable to treat cancers, because of the high risk of infections with antibiotic-resistant bacteria.
A global study estimated that in 2019, almost 5 million deaths occurred with an infection involving antibiotic-resistant bacteria. Some 1.3 million would not have occurred if the bacteria were not resistant.
The UK’s 2014 O'Neill report predicted deaths from antimicrobial resistance could rise to 10 million deaths each year, and cost 2-3.5% of global GDP, by 2050 based on trends at that time.
There is a lot we can do to prevent antibiotic resistance. We can:
raise awareness that many infections will get better by themselves, and don’t necessarily need antibiotics
use the antibiotics we have more appropriately and for as short a time as possible, supported by co-ordinated clinical and public policy, and national oversight
monitor for infections due to resistant bacterial to inform control policies
reduce the inappropriate use of antibiotics in animals, such as growth promotion
reduce cross-transmission of resistant organisms in hospitals and in the community
prevent infections by other means, such as clean water, sanitation, hygiene and vaccines
continue developing new antibiotics and alternatives to antibiotics and ensure the right incentives are in place to encourage a continuous pipeline of new drugs.
Read the other articles in The Conversation’s series on the dangers of antibiotic resistance here.![]()
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Reports this week suggest a near-collision between an Australian satellite and a suspected Chinese military satellite.
Meanwhile, earlier this month, the US government issued the first ever space junk fine. The Federal Communications Commission handed a US$150,000 penalty to the DISH Network, a publicly traded company providing satellite TV services.
It came as a surprise to many in the space industry, as the fine didn’t relate to any recent debris – it was issued for a communications satellite that has been in space for more than 21 years. It was EchoStar-7, which failed to meet the orbit requirements outlined in a previously agreed debris mitigation plan.
The EchoStar-7 fine might be a US first, but it probably won’t be the last. We are entering an unprecedented era of space use and can expect the number of active satellites in space to increase by 700% by the end of the decade.
As our local space gets more crowded, keeping an eye on tens of thousands of satellites and bits of space junk will only become more important. So researchers have a new field for this: space domain awareness.
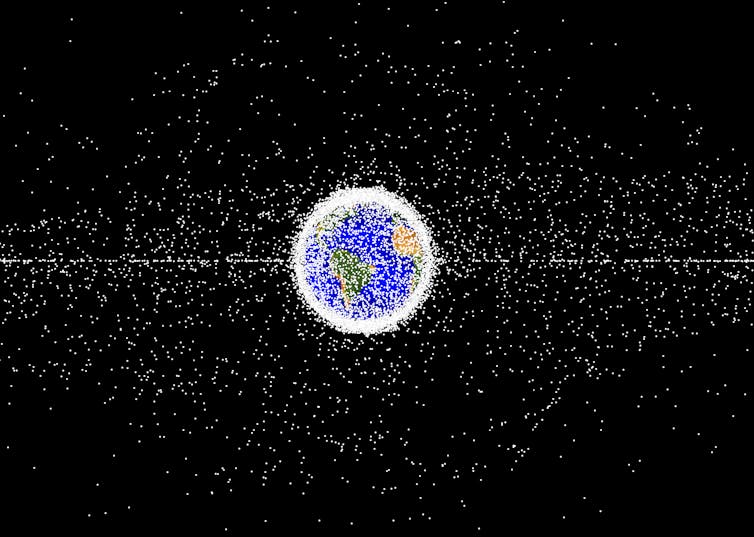
Humans have been launching satellites into space since 1957 and in the past 66 years have become rather good at it. There are currently more than 8,700 active satellites in various orbits around Earth.
Satellites tend to be in three main orbits, and understanding these is key to understanding the complex nature of space debris.
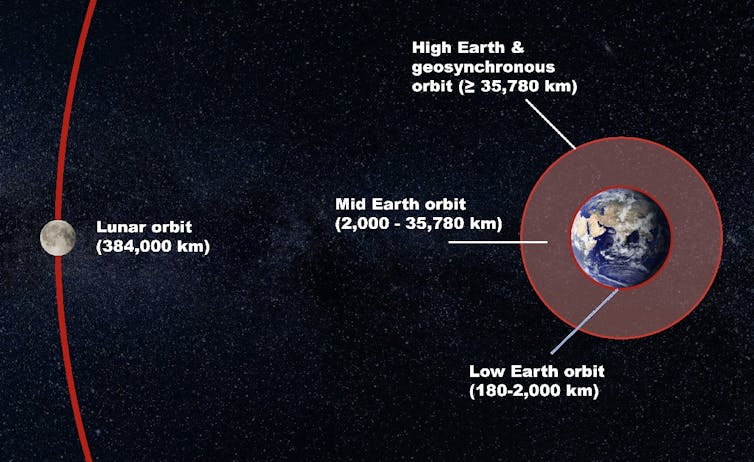
The most common orbit for satellites is low Earth orbit, with at least 5,900 active satellites. Objects in low Earth orbit tend to reside up to 1,000km above Earth’s surface and are constantly on the move. The International Space Station is an example of a low Earth orbit object, travelling around Earth 16 times every day.
Higher up is the medium Earth orbit, where satellites sit between 10,000 and 20,000km above Earth. It’s not a particularly busy place, but is home to some of the most important satellites ever launched – they provide us with the global positioning system or GPS.
Finally, we have very high altitude satellites in geosynchronous orbit. In this orbit, satellites are upwards of 35,000km above Earth, in orbits that match the rate of Earth’s rotation. One special type of this orbit is a geostationary Earth orbit. It lies on the same plane as Earth’s equator, making the satellites appear stationary from the ground.
As you can tell, Earth’s surrounds are buzzing with satellite activity. It only gets more chaotic when we factor in space junk, defined as disused artificial debris in orbit around Earth.
Space junk can range from entire satellites that are no longer in use or working, down to millimetre-wide bits of spacecraft and launch vehicles left in orbit. Latest estimates suggest there are more than 130 million pieces of space debris, with only 35,000 of those large enough (greater than 10cm) to be routinely tracked from the ground.
This is where space domain awareness comes in. It is the field of detecting, tracking and monitoring objects in Earth’s orbit, including active satellites and space debris.
We do much of this with ground-based tracking, either through radar or optical systems like telescopes. While radar can easily track objects in low Earth orbit, higher up we need optical sensors. Objects in medium Earth orbit and geostationary orbit can be tracked using sunlight reflected towards Earth.
For reliable and continuous space domain awareness, we need multiple sensors contributing to this around the globe.
Below you can see what high-altitude satellites can look like to telescopes on Earth, appearing to stay still as the stars move by.
Thanks to our position on Earth, Australia has a unique opportunity to contribute to space domain awareness. The US already houses several facilities on the west coast of Australia as part of the Space Surveillance Network. That’s because on the west coast, telescopes can work in dark night skies with minimal light pollution from large cities.
Furthermore, we are currently working on a space domain awareness technology demonstrator (a proof of concept), funded by SmartSat CRC. This is a government-funded consortium of universities and other research organisations, along with industry partners such as the IT firm CGI.
We are combining our expertise in observational astrophysics, advanced data visualisation, artificial intelligence and space weather. Our goal is to have technology that understands what is happening in space minute-by-minute. Then, we can line up follow-up observations and monitor the objects in orbit. Our team is currently working on geosynchronous orbit objects, which includes active and inactive satellites.
EchoStar-7 was just one example of the fate of a retired spacecraft – the FCC is sending a strong warning to all other companies to ensure their debris mitigation plans are met.
Inactive objects in orbit could pose a collision risk to each other, leading to a rapid increase in space debris. If we want to use Earth’s space domain for as long as possible, we need to keep it safe for all.
Acknowledgment: The authors would like to thank Sholto Forbes-Spyratos, military space lead at CGI Space, Defence and Intelligence Australia, for his contribution to this article.![]()
Sara Webb, Postdoctoral Research Fellow, Centre for Astrophysics and Supercomputing, Swinburne University of Technology; Brett Carter, Associate Professor, RMIT University, and Christopher Fluke, SmartSat Professorial Chair, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.